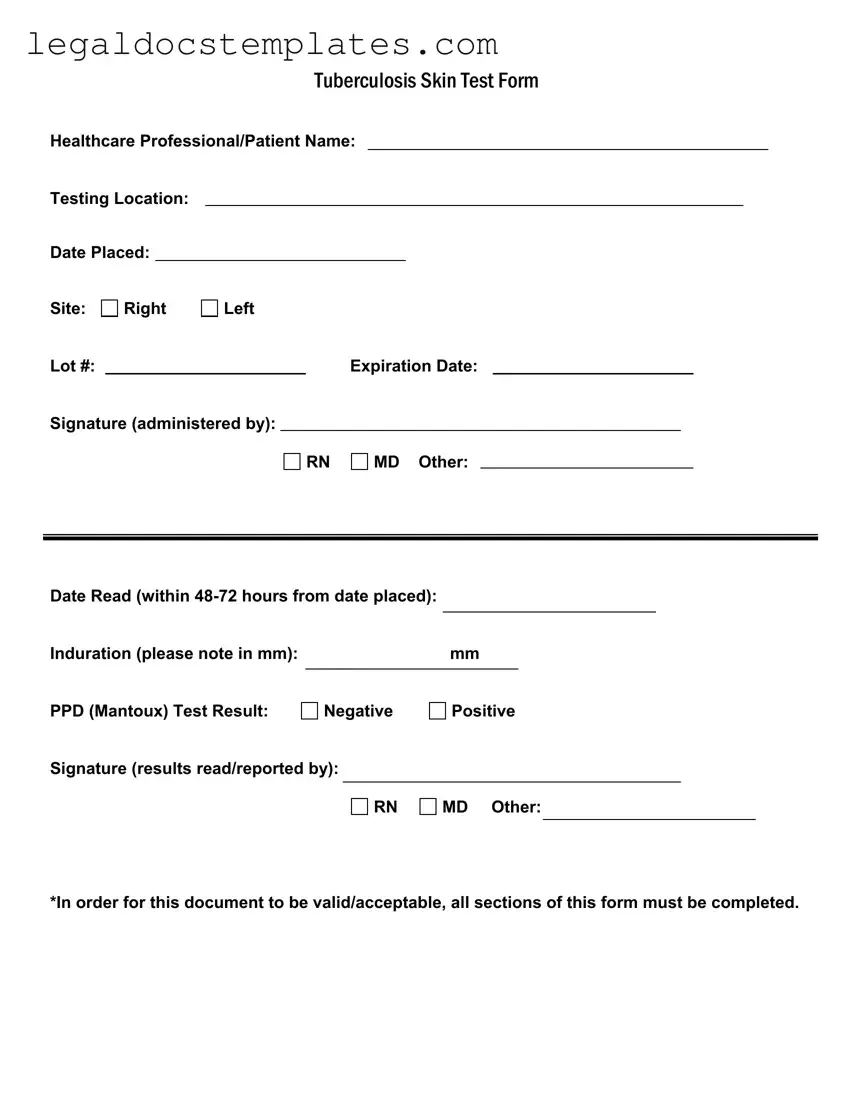
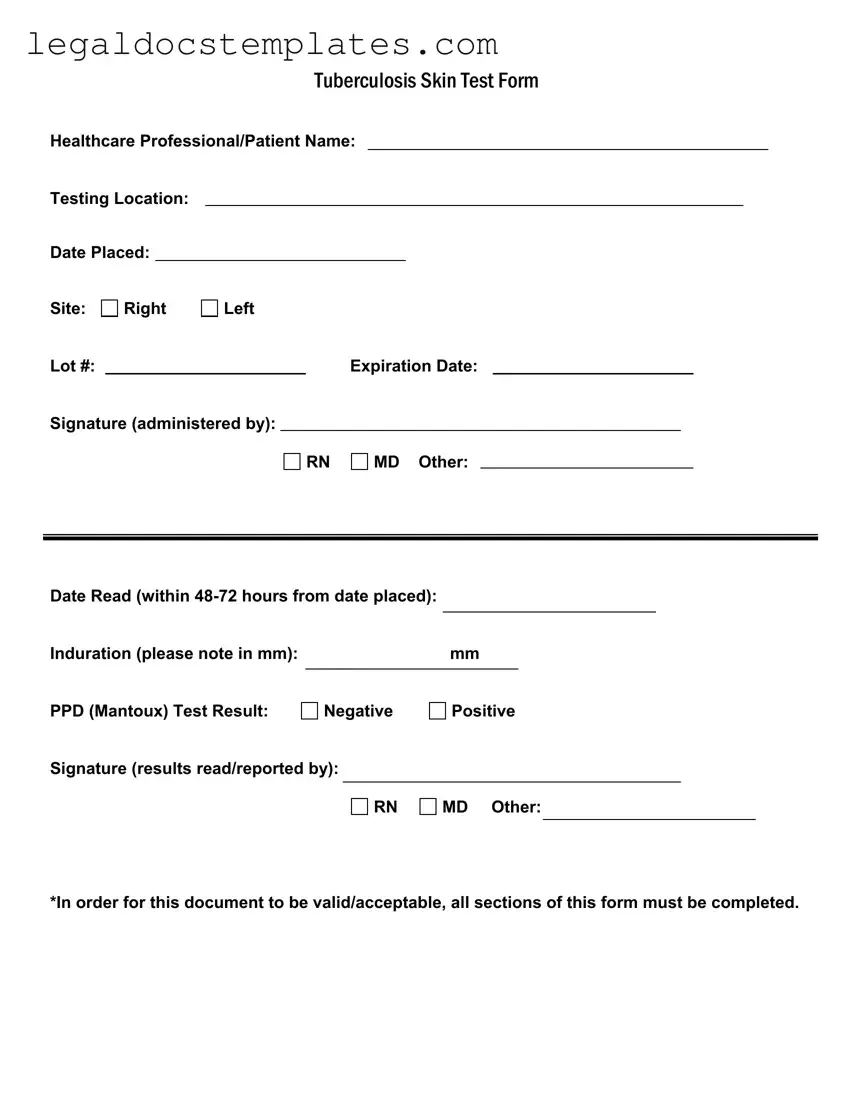
The TB Test Form, also known as the Tuberculosis Skin Test Form, is a document used by healthcare professionals to record the details and results of a tuberculosis (TB) skin test. This test determines if someone has been exposed to TB bacteria. The form includes sections for the patient's name, testing location, dates related to the test, the site of the injection (right or left arm), the lot number of the test substance, the expiration date of that substance, and signatures from the professionals administering and reading the test. Additionally, the form requests the measurement of induration (swelling) in millimeters and the final test result.
Who can administer and read the TB Skin Test?
The administering and reading of a TB Skin Test must be done by qualified healthcare professionals. According to the form, those authorized include Registered Nurses (RN), Medical Doctors (MD), and other certified individuals under respective healthcare regulations. Both the administration and reading of the test require signatures from these professionals to validate the form.
When should the TB Skin Test be read?
The TB Skin Test results should be read between 48 to 72 hours after it's been placed. Reading the test within this timeframe is crucial for accurate results, as the reaction site, where the test was injected, needs to be examined for swelling or induration to determine if the test is positive or negative.
On the TB Test Form, induration refers to the swollen, raised area at the test site and is measured in millimeters. The size of the induration is a key factor in determining the test result. Generally, larger indurations indicate a positive result, suggesting exposure to TB bacteria, but interpretation guidelines can vary based on the patient's risk factors and history. Health professionals use these measurements alongside other information to assess an individual's TB exposure.
A positive result on a TB Test Form suggests that the person has been exposed to the TB bacteria and has developed an immune response. It is important to note that a positive result does not necessarily mean the individual has active tuberculosis; further testing, such as a chest X-ray or a sputum test, may be required. A negative result indicates that no significant reaction was observed, suggesting no exposure to the bacteria or an immune system that did not respond to the test.
Yes, completing all sections of the TB Test Form is essential for it to be valid. Incomplete forms may not be accepted as they lack crucial information needed for accurate interpretation and record-keeping. Each section, including signatures from the healthcare professionals, contributes to the documentation's integrity and ensures the test's results are accurately reported.
It's advisable to keep the TB Test Form for as long as recommended by health regulations or by your healthcare provider. These documents can serve as important medical records, providing a history of TB exposure or clearance, especially for individuals who require regular testing due to their profession or health status. In many cases, keeping records for a minimum of a few years is recommended, but it's best to consult with a healthcare professional for guidance specific to your situation.