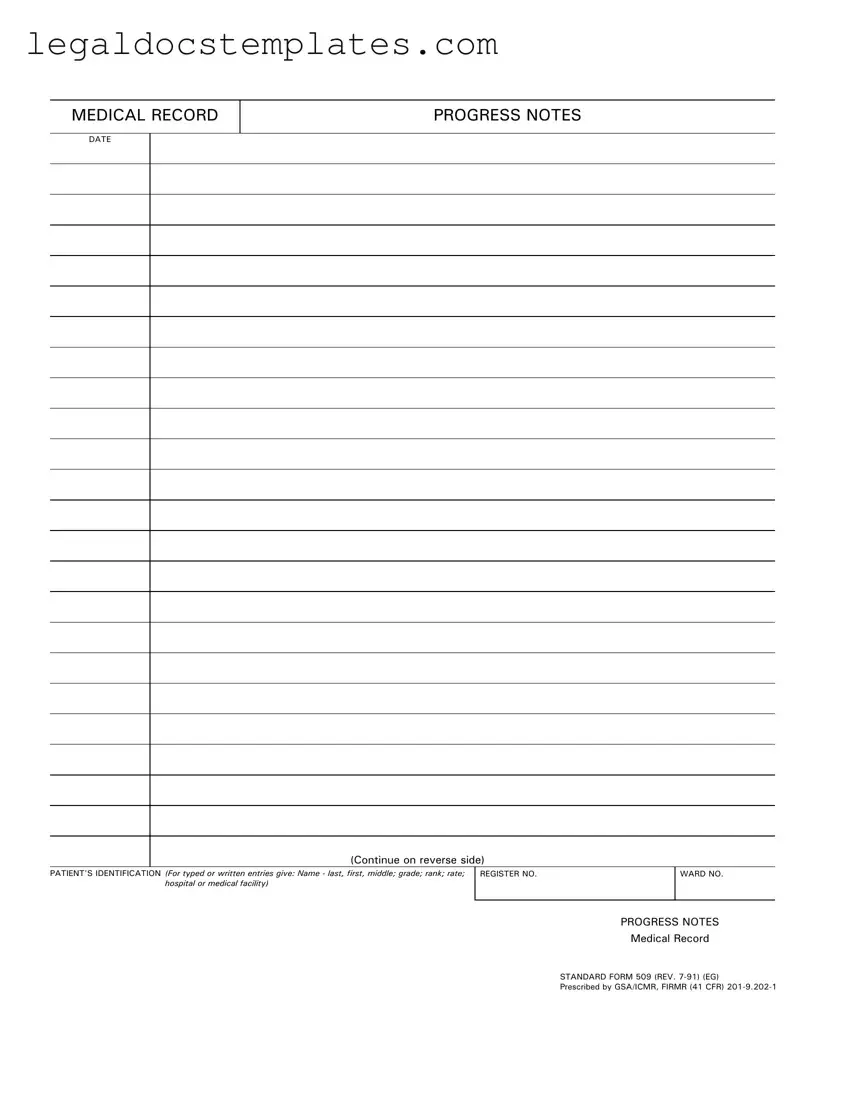
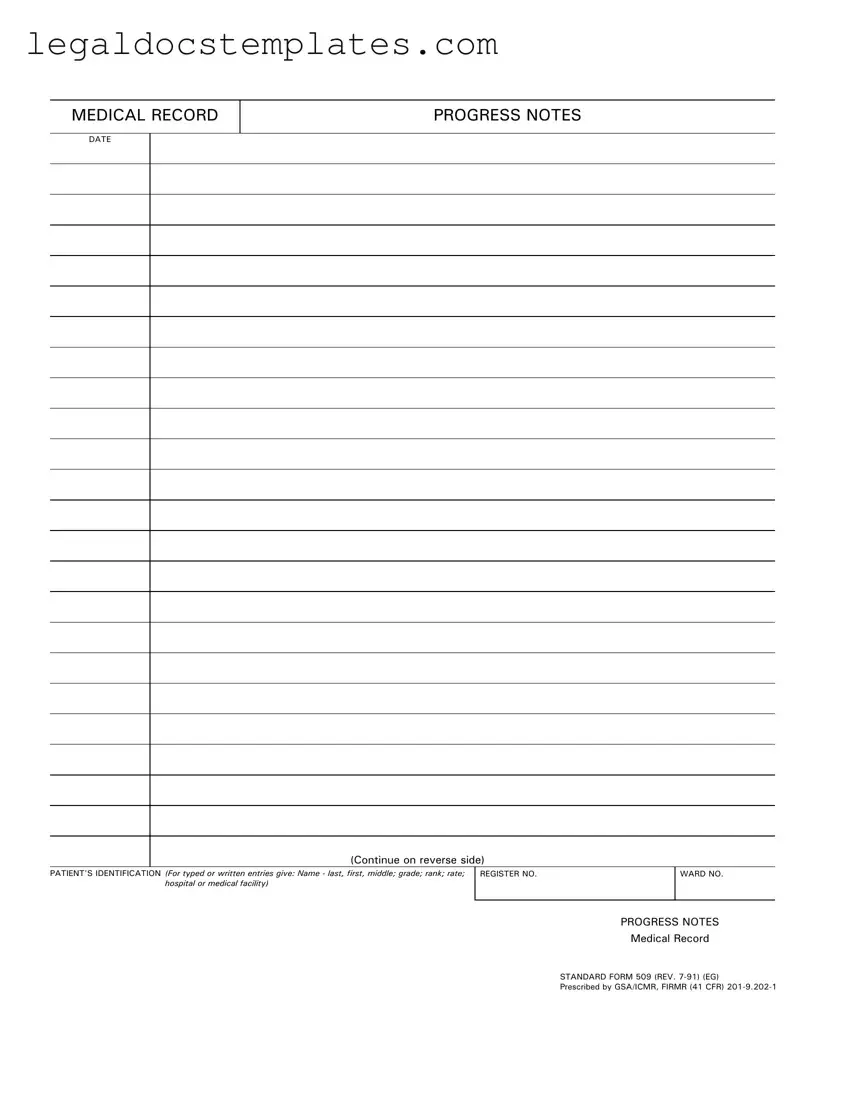
Fill Out Your Progress Notes Template
A Progress Notes Form is a crucial document used in the medical field to record the care and condition of a patient over time. It includes essential details such as patient identification, medical history, updates on the patient's condition, treatments administered, and the healthcare provider's observations. If you are currently managing patient care or need to update medical records, ensure accurate documentation by clicking the button below to fill out the Progress Notes Form.
Access Progress Notes Now
Fill Out Your Progress Notes Template
Access Progress Notes Now
Access Progress Notes Now
or
⇩ PDF Form
Don’t spend hours on this form
Complete Progress Notes online in minutes, fully digital.