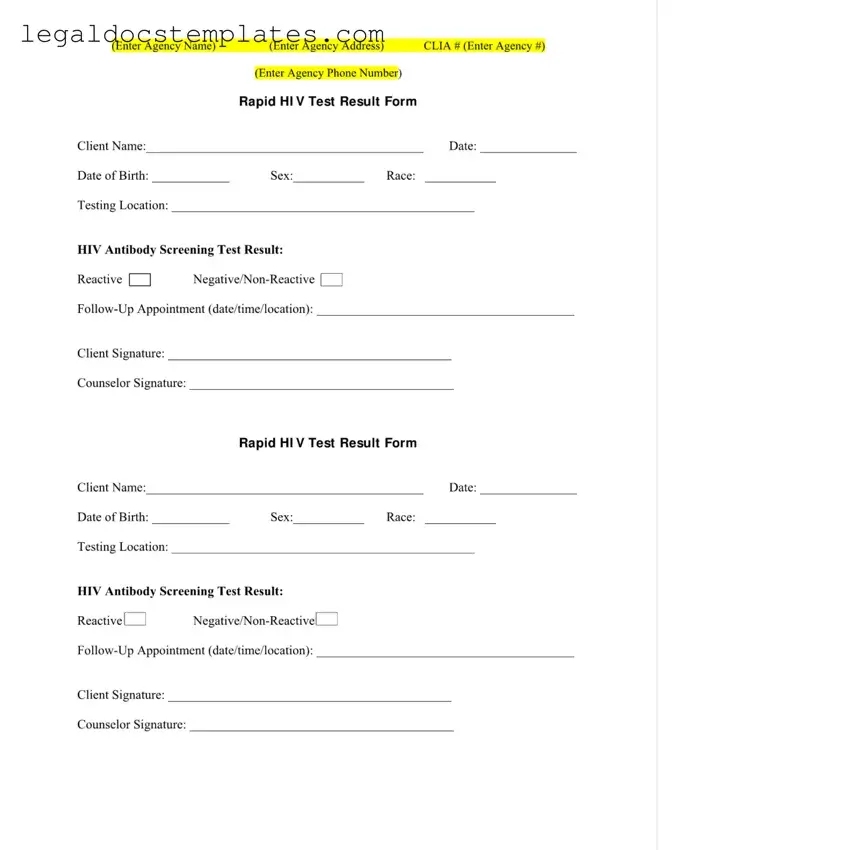
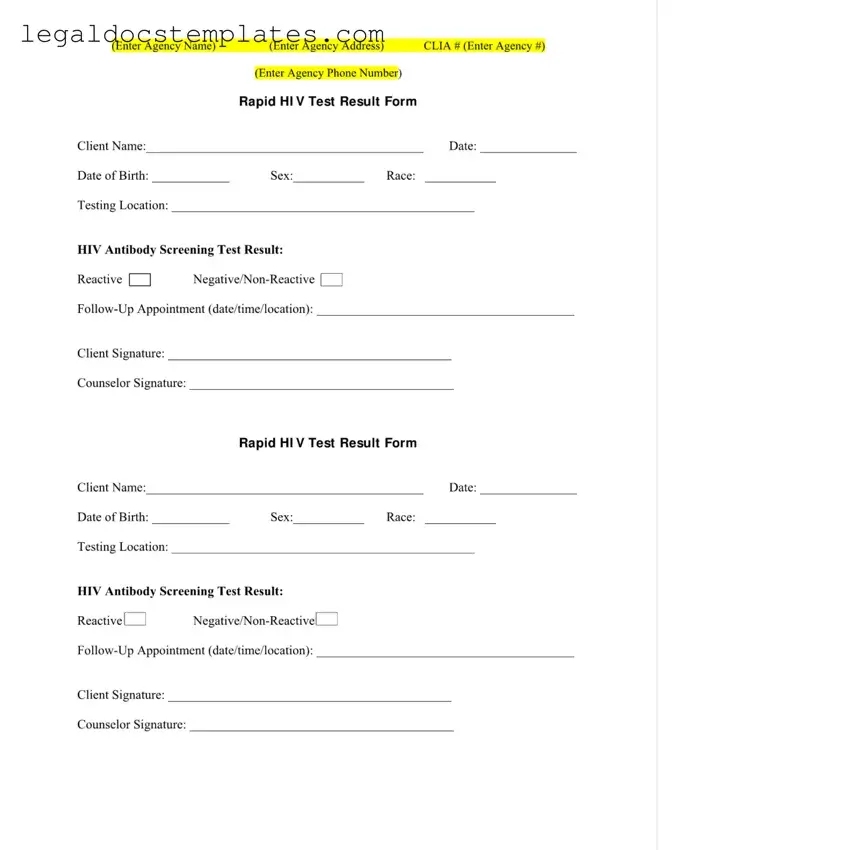
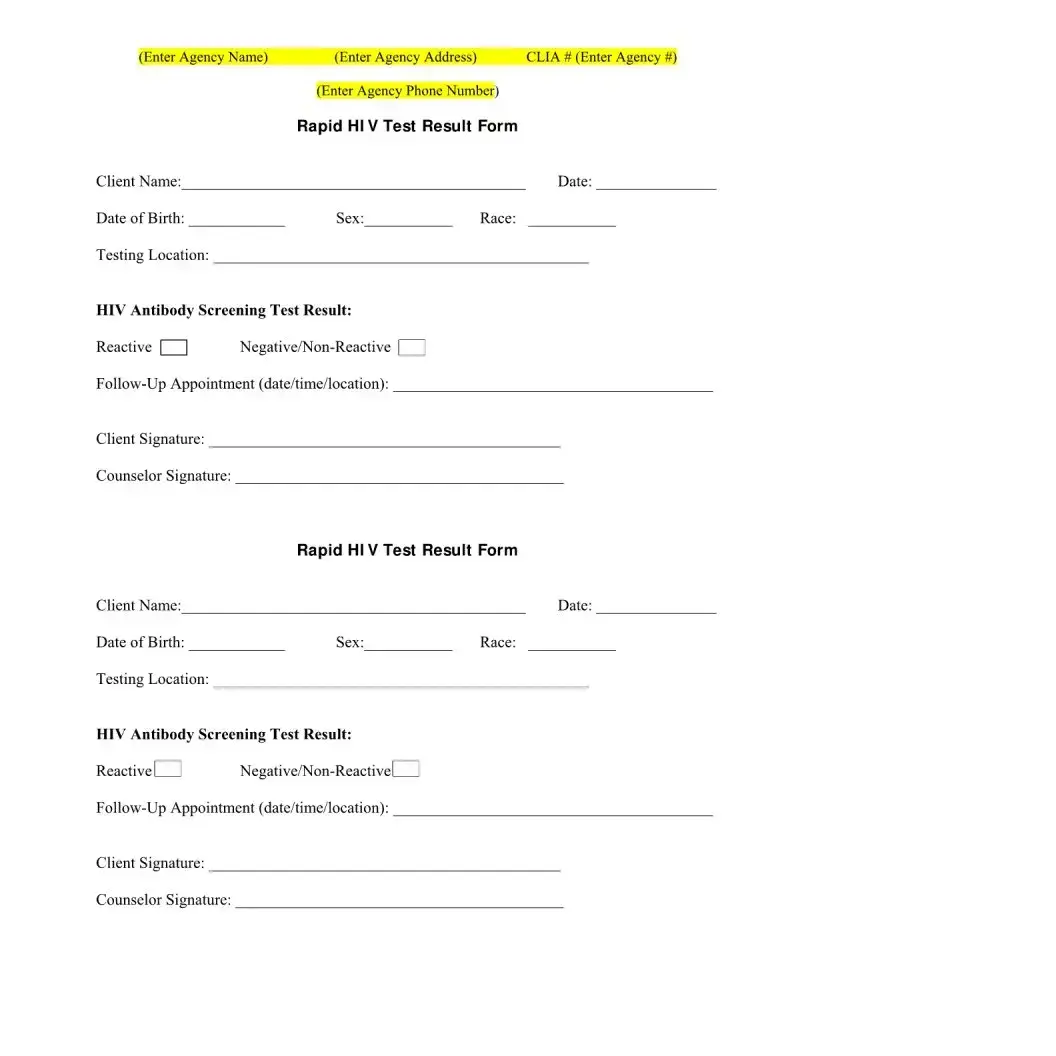
A Negative HIV Test Form is similar to a Positive HIV Test Form in that both are critical in the medical documentation of an individual's HIV status and facilitate follow-up care. While the Negative HIV Test Form confirms the absence of HIV antibodies at the time of testing, ensuring the individual that they do not currently have HIV, the Positive HIV Test Form indicates the presence of these antibodies, signaling an HIV infection. Both forms require client and counselor signatures, solidifying the test's validity and the understanding of its outcome. Moreover, these documents prompt necessary actions - counseling and medical follow-ups, albeit in different directions based on the results.
Comparable to the Vaccine Administration Record, the Negative HIV Test Form documents a specific healthcare interaction focused on preventative care. The Vaccine Administration Record tracks the administration of a vaccine, its type, dose, and the date given, similar to how the HIV Test Form records the administration of an HIV test, its result, and the testing date. Both forms serve as an official record of the patient's health intervention and follow a similar structure of documentation, ensuring the patient's health care narrative is accurately and comprehensively captured.
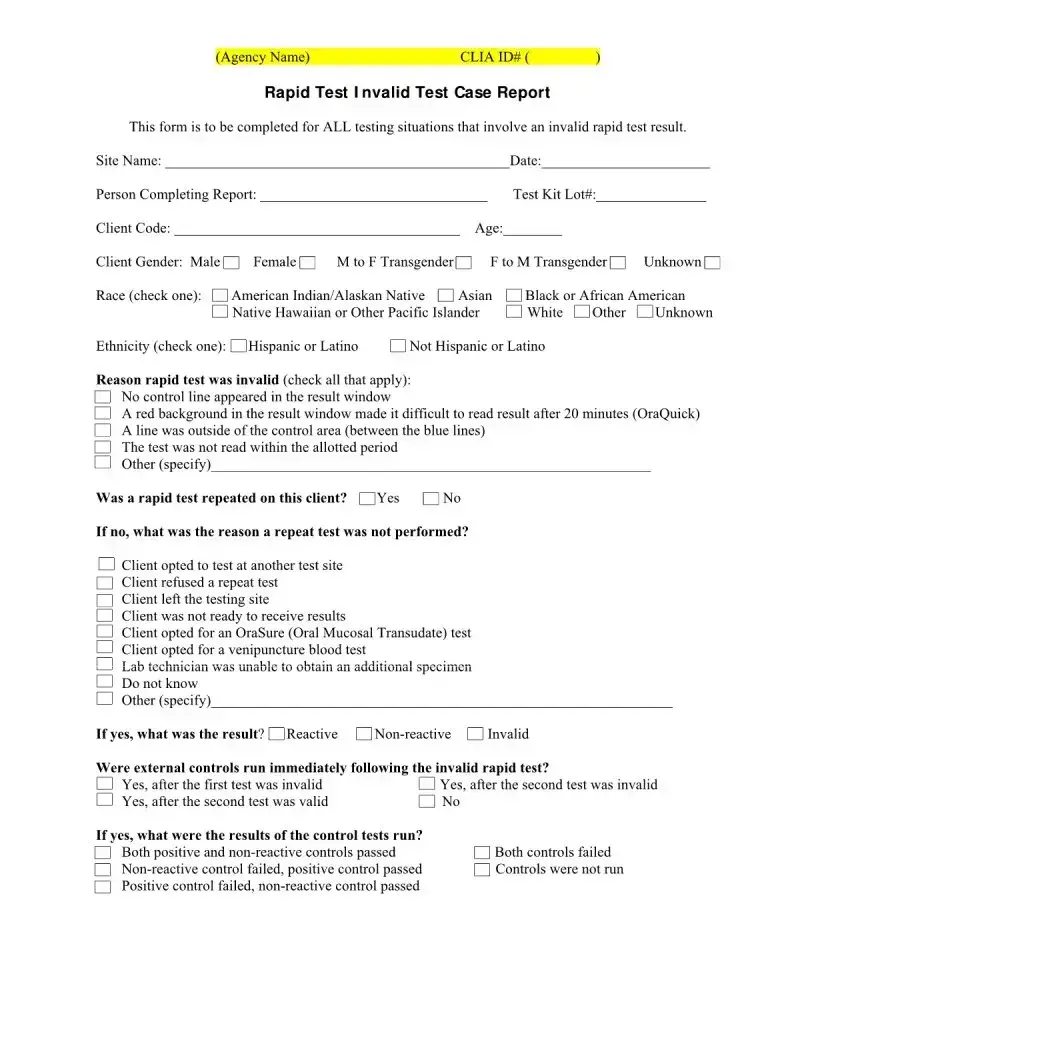
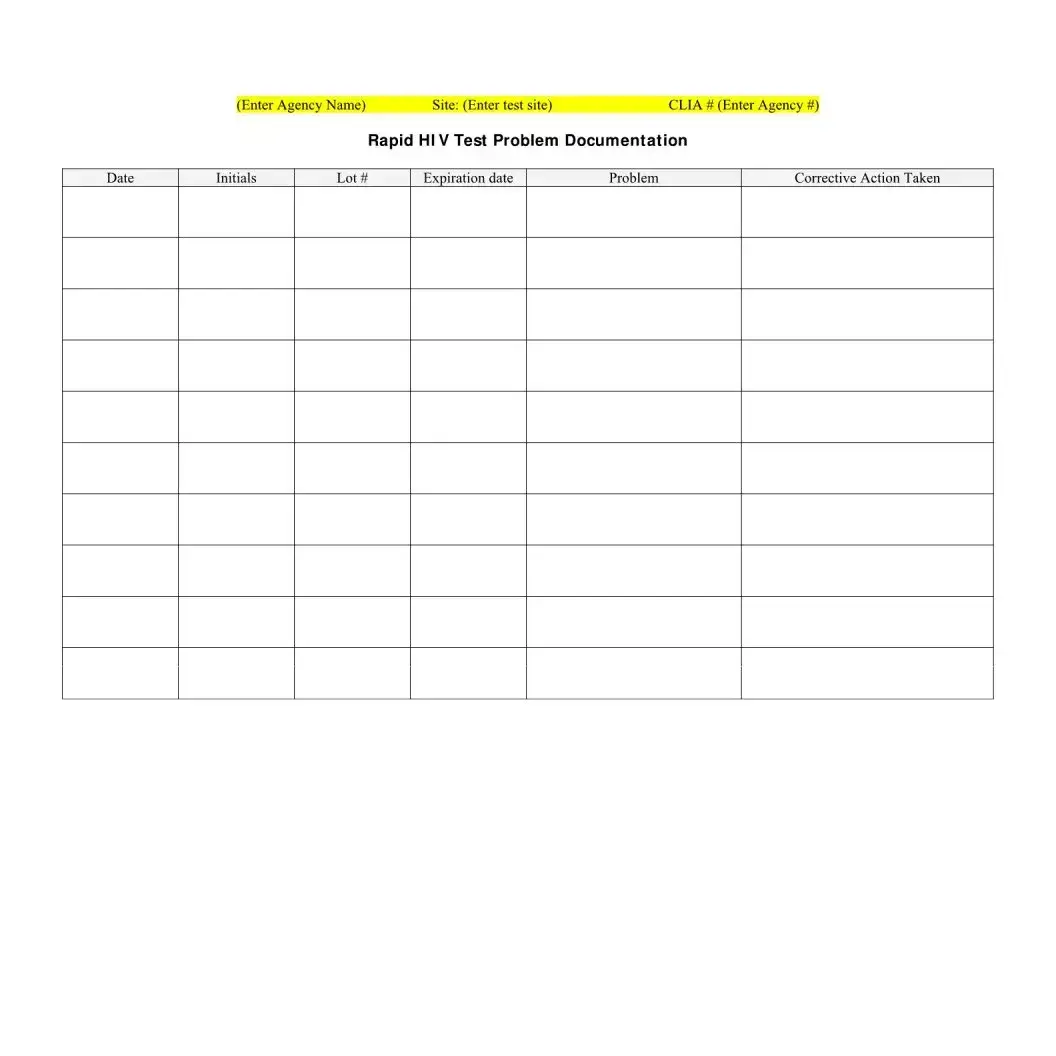
The Laboratory Test Result Form shares similarities with the Negative HIV Test Form in its purpose of documenting and communicating specific test outcomes. Both types of documents detail the examination done, the results, and usually include a section for follow-up actions. While the Laboratory Test Result Form can cover a broad range of tests (from blood counts to metabolic panels), the HIV Test Form is specific to HIV status. They both contribute significantly to patient care by informing further clinical decisions and patient counseling.
The Medical Consent Form, like the Negative HIV Test Form, requires the signature of the client to acknowledge the procedure that has been or will be undertaken. Both documents are integral in ensuring that the individual has been informed of their health status or the medical procedure's nature and consents to it. Though one is specific to HIV testing and the other can apply to various medical procedures, each upholds the principle of informed consent in healthcare.
Similarly, the Patient Intake Form aligns with the Negative HIV Test Form as it gathers essential information at the outset of a healthcare service. While the Patient Intake Form collects general health history, current symptoms, and personal information, the HIV Test Form focuses on HIV-specific data, such as the test result and follow-up. Both forms mark the beginning of a care process, providing a basis for personalized medical attention and facilitating optimal health outcomes.
The Medication Log Sheet, used to document the prescription, administration, and effect of medications on a patient, bears resemblance to the Negative HIV Test Form in its role of tracking a specific aspect of patient care. Although one focuses on medication and the other on HIV testing, both are pivotal in maintaining a detailed healthcare record, ensuring compliance with the treatment plan, and evaluating the efficacy of medical interventions.
The Sexual Health History Form, which outlines an individual's sexual behavior, contraception use, and history of sexually transmitted infections (STIs), is akin to the Negative HIV Test Form in its focus on sexual health. Both forms are tools in assessing risks, diagnosing conditions, and planning appropriate interventions regarding sexual health. They play critical roles in preventive healthcare, aiming to manage or avert potential health issues through comprehensive history-taking and testing.
An Appointment Reminder Card, while not as detailed as the Negative HIV Test Form, similarly serves the purpose of guiding patients through their healthcare journey. While the reminder card prompts patients about upcoming appointments, ensuring continuity of care, the Negative HIV Test Form also incorporates a section for follow-up appointments, emphasizing the importance of ongoing care and monitoring after the HIV test result is known.
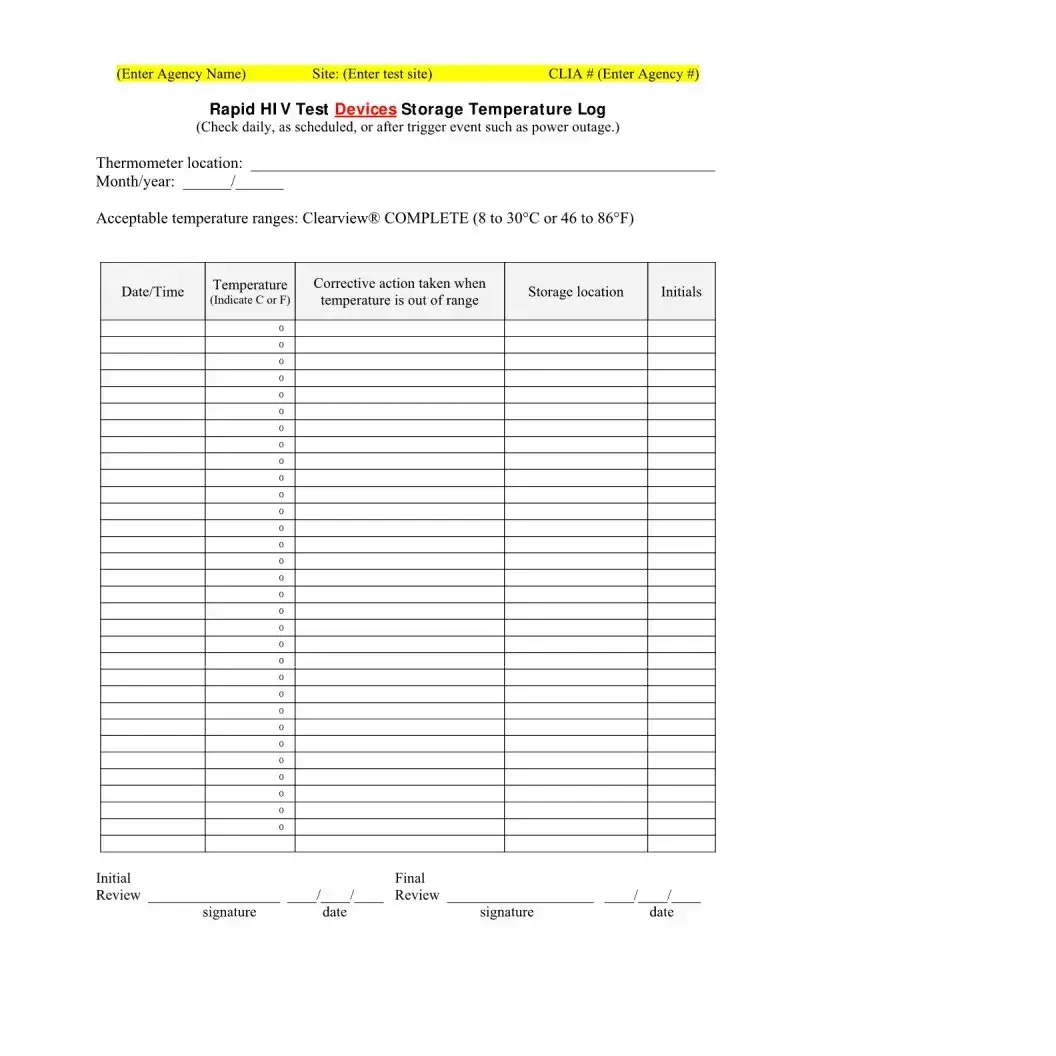
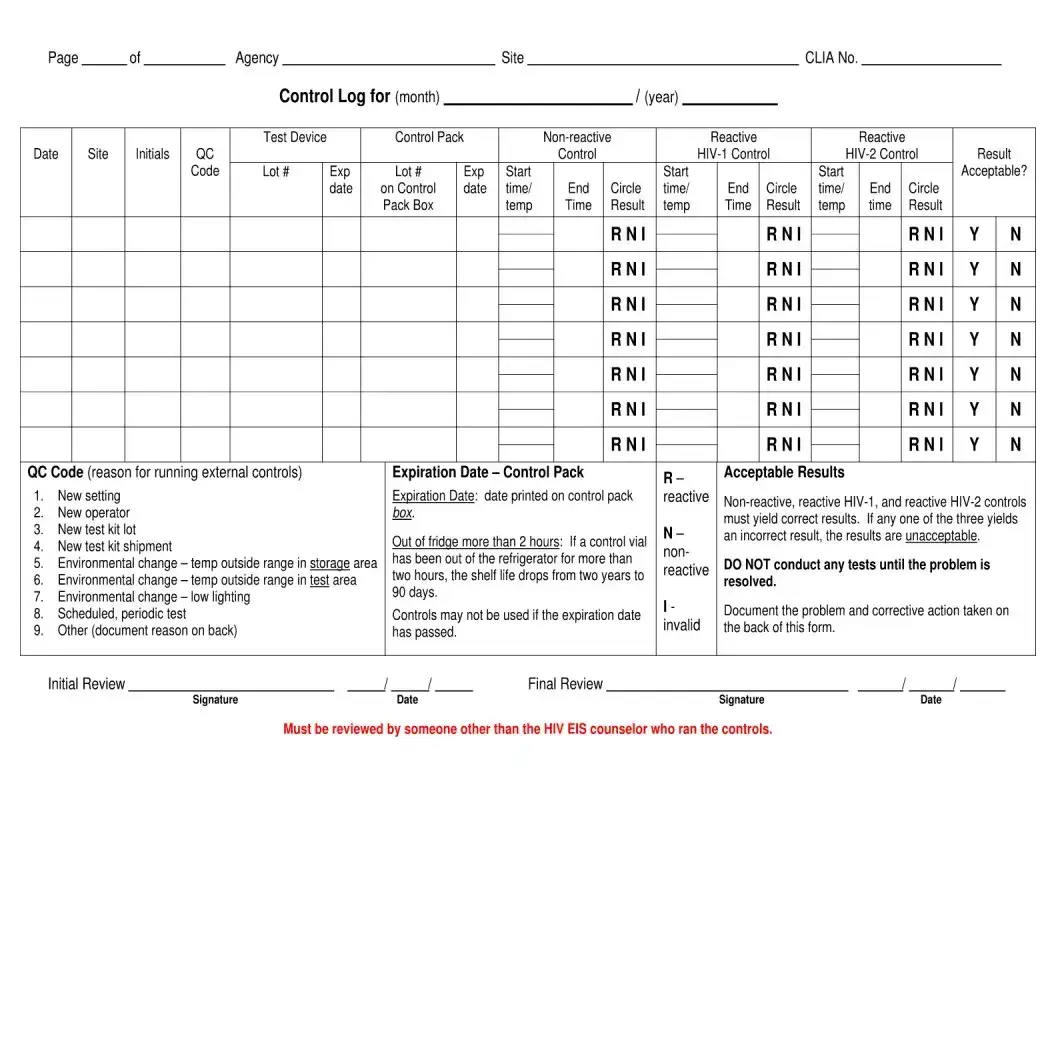
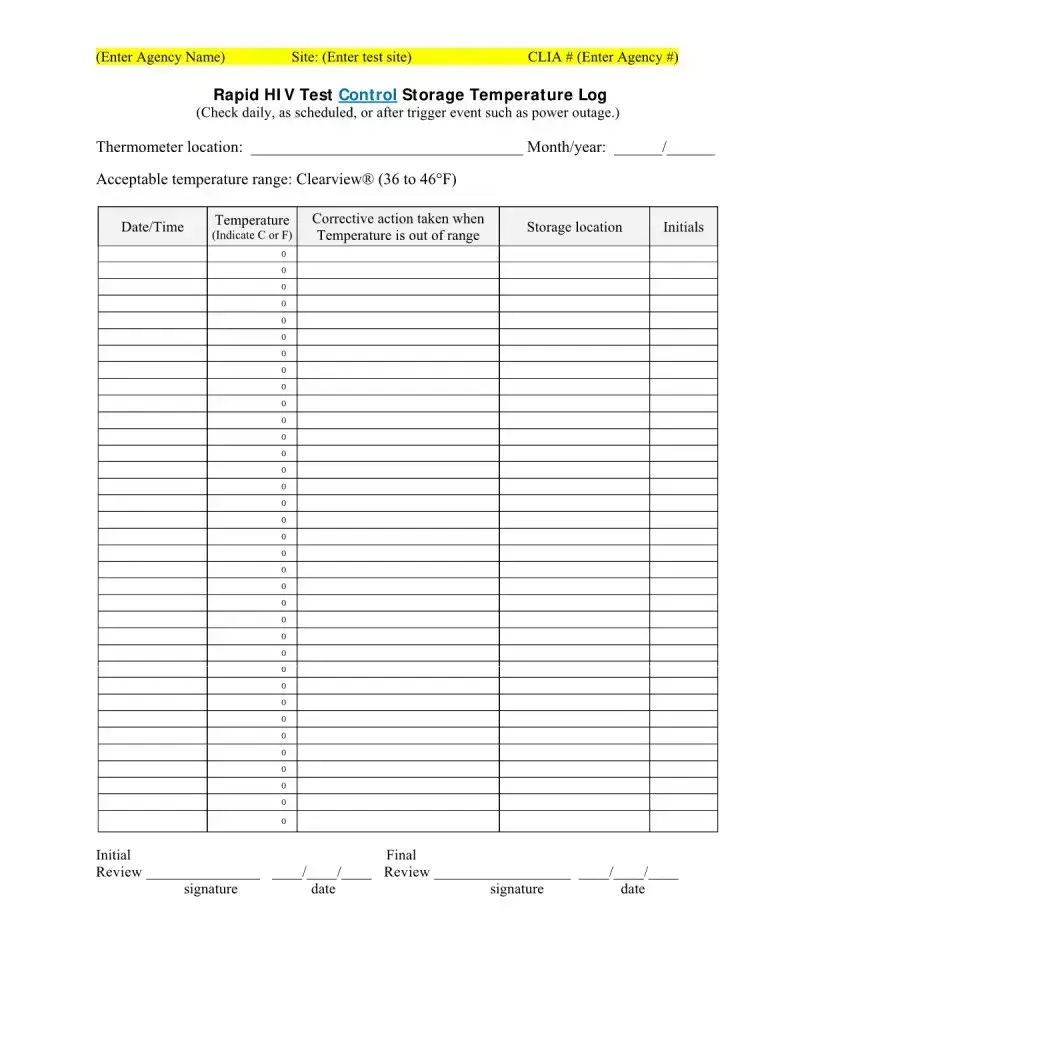
The Temperature Log Sheet, used for monitoring and documenting the temperature of medical storage units, shares its preventive care goal with the Negative HIV Test Form. The Temperature Log Sheet ensures that vaccines, medications, and test devices like HIV test kits are stored within safe temperature ranges to maintain their efficacy. This form, by ensuring the integrity of medical supplies, indirectly supports accurate healthcare testing and treatment, just as the HIV Test Form directly documents the outcome of such tests.
The Consent for Telehealth Consultation Form parallels the Negative HIV Test Form in its adaptation to modern healthcare needs, facilitating services through non-traditional means. While the Telehealth Consent Form documents agreement to receive health care services via telecommunications technologies, the HIV Test Form adapts to current health challenges by documenting critical test results. Both forms reflect contemporary approaches to providing and documenting healthcare, ensuring patient engagement and care continuity amidst evolving healthcare landscapes.