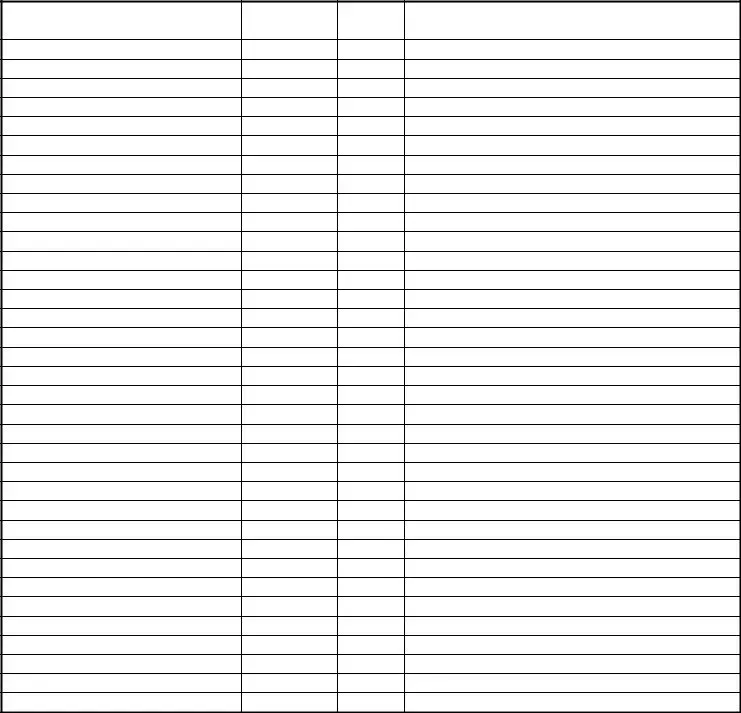
The Medication Count Sheet form closely resembles a Narcotic Log. Both documents track the administration of sensitive medications to individuals under care. They detail the quantity of medication on hand, dosages administered, and the resulting quantities remaining, ensuring accountability and compliance with regulatory requirements. The primary difference lies in the Narcotic Log's specific focus on controlled substances.
Similarly, a Medication Administration Record (MAR) shares many features with the Medication Count Sheet. The MAR is comprehensive, documenting not only the medication given but also the time, dose, and individual who administered it. This record serves as a critical component in healthcare settings, providing a chronological account of a patient's medication management, essential for ensuring proper care and treatment continuity.
A Patient Care Report (PCR) is another document that parallels the Medication Count Sheet in its function of documenting care provided to individuals, albeit in a more holistic manner. PCRs are used by emergency medical services to record all aspects of patient care, from the initial assessment to the medications administered, including the specifics captured in a Medication Count Sheet, ensuring a thorough account of the patient's treatment and condition during transport.
A Controlled Substance Inventory Log is akin to the Medication Count Sheet but focuses explicitly on tracking the stock levels of controlled substances within healthcare facilities. It lists quantities received, dispensed, wasted, and remaining in stock. This meticulous tracking ensures compliance with laws regulating these potent medications, preventing misuse and diversion.
An Inventory Management Record, while not exclusive to healthcare, resembles the Medication Count Sheet in its purpose to monitor the flow of inventory - in this case, medication. It tracks items' availability, reorder levels, and quantities on hand, ensuring that operations proceed smoothly and without interruption due to shortages.
The Treatment Administration Record bears similarities to the Medication Count Sheet, with a focus on documenting all treatments administered to patients, including but not limited to medications. It captures details such as treatment type, dose, and administration time, playing an essential role in coordinating patient care and monitoring treatment effectiveness.
A Pharmacy Dispensing Log is closely related to the Medication Count Sheet, specifically in its function of recording medications dispensed to patients or care facilities. This log ensures accuracy in dispensing, tracks inventory, and helps in preventing medication errors by providing a clear record of what has been provided to whom and in what quantity.
Lastly, the Medication Reconciliation Form shares a goal with the Medication Count Sheet - ensuring accurate and safe medication use. This form is used when patients transition between care settings, documenting all medications a patient is taking to prevent duplications, omissions, or interactions. It ensures continuity and safety in medication administration across different care environments.