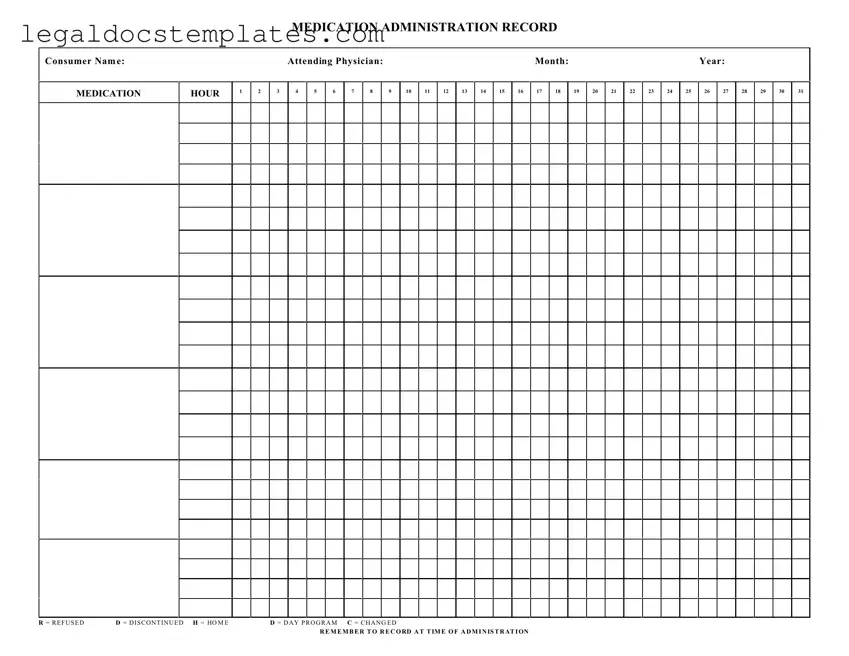
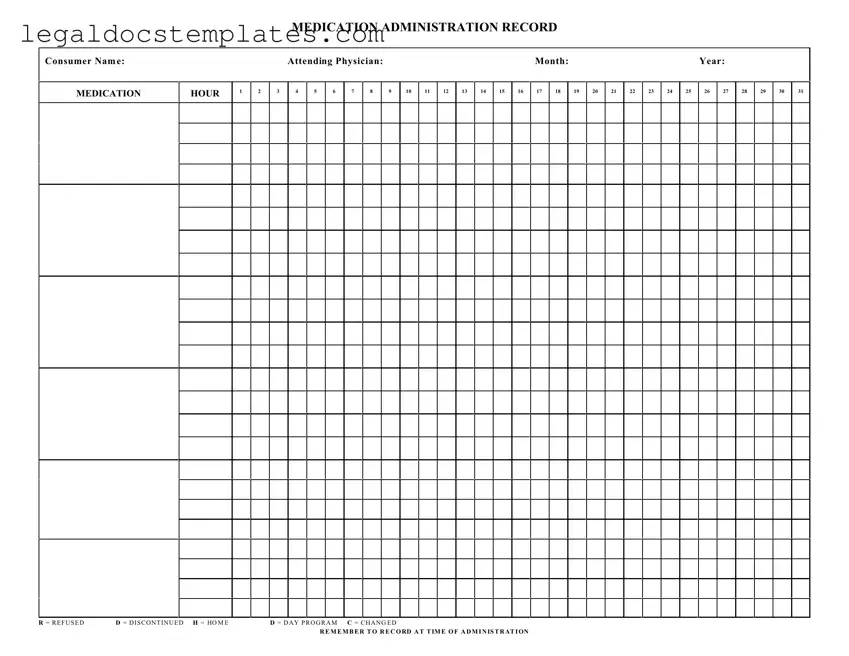
One common mistake made when filling out the Medication Administration Record Sheet (MAR) is overlooking the correct recording of the date and time of medication administration. The form provides columns for each day of the month to meticulously track the administration times. However, individuals sometimes mark the medication as administered without specifying the exact time, leading to confusion and potential gaps in medication management. This oversight can hinder the accuracy of the medication regimen and compromise the consumer's health.
Another error involves the incorrect notation or omission of medication changes. The MAR uses specific codes such as R for refused, D for discontinued, and C for changed. These codes play a crucial role in the history of the consumer's medication regimen. Unfortunately, caretakers may fail to update the form when a medication is discontinued or changed, or they might use the wrong code. This mistake can lead to the administration of incorrect dosages or the wrong medication altogether, posing significant risks to the consumer's well-being.
There's also a tendency to misunderstand the attending physician's instructions, leading to errors in medication administration. The MAR requires clarity in the execution of the physician's orders, including the precise dosage and timing. Misinterpretation of these instructions can result in administering the wrong dose or administering it at incorrect times, potentially causing harm to the consumer. It is crucial to double-check the doctor's orders and clarify any ambiguities before documenting and administering medications.
Errors in recording the consumer's name and identifying information on the MAR can lead to critical administration errors. The sheet starts with sections for the consumer's name, the attending physician, month, and year, which must be accurately filled in to ensure the medication is administered to the correct individual. Caregivers sometimes rush through this step or assume the information is already known, which can lead to medication mix-ups, especially in settings where multiple consumers are being cared for.
Forgetting to document when a consumer refuses medication is another mistake that can occur. The MAR provides an R code specifically for this situation. Documentation of refusal is vital for legal and health reasons, as it indicates that the consumer chose not to take the medication at a particular time. Without this information, there might be unwarranted assumptions about non-compliance or missed doses, which can complicate the consumer’s health management plan.
Not marking the medication administration setting on the MAR is another oversight. The sheet distinguishes between different administration settings, such as home (H), day program (D), etc. This distinction is essential for coordinating care across multiple settings, ensuring continuity and accuracy in medication administration. Failing to indicate the correct setting can lead to confusion and errors in the continuity of care.
Lastly, individuals sometimes neglect the importance of timely and accurate record-keeping on the MAR. Delayed entries or retrospective documentation can compromise the integrity of the medication administration record. It is imperative to record the medication administration at the time it occurs. This practice ensures the reliability of the record and the safety of the medication administration process, reinforcing the overarching goal of maintaining the consumer’s health and safety.